Many expectant parents eagerly anticipate learning the sex of their baby, either with a fetal ultrasound, a cell-free DNA (cfDNA) test, or a combination of both. Yet in rare instances, a mismatch in test results may appear in an estimated one in 1,500-2,000 pregnancies, prompting understandable distress and confusion for your patient. Understanding the possible reasons for the divergent findings can inform clinical decision-making and soothe worried parents-to-be.
Reliable Methods for Sex Identification
Ultrasound and cfDNA testing are both reliable methods of determining fetal sex. Prenatal DNA screening provides accuracy above 99 percent in tests performed after the 10th week of pregnancy. Similarly, ultrasound is more than 99 percent accurate in identifying male and female sex organs in the second trimester of pregnancy. In the first trimester, ultrasound offers 86 percent accuracy in determining the sex of a female fetus and 69 percent accuracy with a male.
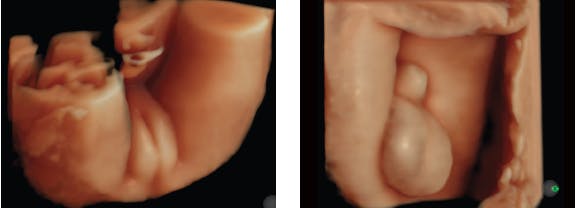
During the late first trimester and early second trimester, ultrasound aids in sex identification based largely on the direction of the genital tubercle or sagittal sign. An upward direction of the tubercle indicates a male fetus while a downward direction suggests a female. In contrast, sonographic determination in the late second trimester relies on direct visualization of fetal external genitalia. Other anatomical landmarks, such as the fetal scrotum, labial lines, and uterus, may inform the evaluation, but malformed genitalia may lead to an inaccurate conclusion.
At the same time, underlying factors may affect the reliability of a blood test for cfDNA. For example, unexpected sources of DNA in maternal blood—such as from a vanishing twin or maternal organ transplant—may produce results that don't reflect the true sex of the developing fetus. What's more, unforeseen genomic alterations of the Y chromosome can hinder sex evaluation in both fetal ultrasound and cell-free DNA testing.
Mosaicism is one such example. Mosaicism arises when a portion of cells in the fetus or placenta, or both in some cases, possess a Y chromosome while the rest do not. Depending on severity of mosaicism and the location, the test may or may not detect the Y chromosome. Likewise, external male genitalia may appear or may not be seen during ultrasound screening.
Deletions of the Y chromosome may also interfere with the detection of Y chromosome sequences in a cell-free DNA test, sometimes producing a result suggesting a female fetus with male external genitalia. Yet, when the sex-determining region on the Y (SRY) gene is deleted, the fetal external genitalia appear female on ultrasound, although a DNA test suggests the fetus is male because it's picking up other Y chromosome sequences. A variety of single-gene disorders, isolated malformations, genetic syndromes, and chromosomal anomalies also may cause ambiguous genitalia or divergent test results.
Health History Review
A careful health history may inform whether an ultrasound assessment should be offered before cfDNA testing to prevent possible testing discrepancies. Factors to consider include a prior organ transplant, exposure to virilizing medications, and fetal demise in a pregnancy with multiples. This is particularly the case with fetal demise in a multiple pregnancy, which may lead to an inaccurate finding. In such instances, sonographic assessment might be recommended ahead of cfDNA testing, aiding the identification of a deceased or vanishing twin.
A detailed second-trimester ultrasound may also resolve questions about the sex of the fetus while evaluating for possible fetal abnormalities. Prenatal diagnostic testing may also be considered in consultation with your patient, with options that include karyotype, microarray, single-gene disorder panels, or exome sequencing.
A Multidisciplinary Approach
Early detection of fetal sex discordance is crucial as it may point to an underlying chromosomal, genetic, or biochemical condition, allowing for prompt postnatal treatment. Supportive counselling can help address expectant parents' concerns and relieve anxiety throughout the evaluation process and beyond.
When cfDNA testing and ultrasound imaging produce opposing results, a multidisciplinary team approach may be part of standard clinical recommendations. The team may include genetic counsellors and maternal-fetal medicine physicians, along with postnatal evaluations by specialists in neonatology, endocrinology, and urology. Together, the multidisciplinary team provides an avenue for clearer understanding of the root cause of the discordance, while collectively promoting maternal and fetal health during pregnancy and after delivery.
Interested in learning more? Click HERE.